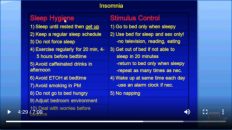
美国医学院医生清晰讲解如睡眠卫生(sleep hygiene)和失眠刺激管控(stimulus control)失败后,应对病人实施新的失眠疗法,包括放松疗法(relaxation technique)、睡眠限制(sleep restriction)、行为疗法(behavioral therapy)、认知疗法(cognitive therapy)和行为-认知疗法(behavioral-cognitive therapy)。
CBTI Stimulus Control, Sleep Hygiene Continued
Welcome to another MedCram lecture. We’re going to talk about behavioral therapy in relation to insomnia. We already talked earlier about the general approach. We want to look for diseases. We want to do sleep hygiene and stimulus control. The other thing we want to do is behavioral therapy. This is what we do if sleep hygiene and stimulus control don’t work. The current recommendation is that we do it in conjunction with medication, but let’s talk about these separately.
欢迎参加另一个MedCram讲座。我们将讨论与失眠有关的行为疗法。前面我们已经讨论了通用方法。我们想寻找疾病。我们想做睡眠卫生和刺激控制。我们要做的另一件事是行为疗法。如果睡眠卫生和刺激控制不起作用,这就是我们要做的。当前的建议是我们将其与药物结合使用,但让我们分别讨论这些。
Here’s another way of looking at it, again a little bit cleaner. Our general approach is we look for diseases, do hygiene handout and the stimulus control. If that doesn’t work, we move on to a combination of behavioral therapy and medication. We will deal with these separately, but we’ll deal with behavioral therapy first.
这是另一种看待方式,也更加干净。我们的一般方法是寻找疾病,进行卫生分发和控制刺激。如果那不起作用,我们将进行行为疗法和药物治疗的结合。我们将分别处理这些问题,但是首先将处理行为疗法。
What we’re going to talk about are the four different behavioral therapies: relaxation technique, sleep restriction therapy, cognitive therapy, and then cognitive-behavioral therapy. The medications that we’ll talk about in a later lecture are the benzodiazepines, nonbenzodiazepine sedatives, the melatonin agonists, and then finally the antidepressants.
我们将要讨论的是四种不同的行为疗法:放松技术,睡眠限制疗法,认知疗法,然后是认知行为疗法。我们将在以后的讲座中讨论的药物是苯二氮卓类药物,非苯二氮卓类镇静剂,褪黑激素激动剂,最后是抗抑郁药。
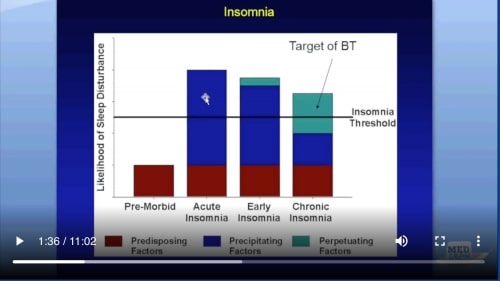
So the purpose of behavioral therapy, if you’ll recognize this graph, now little cleaned up here, is in the premorbid state, we had these predisposing factors which remained throughout our lifetime, and then sometimes these precipitating factors would occur that would take us over the insomnia threshold. When that occurred, even though that actual precipitating factor would go down below that insomnia threshold, the problem was is that we unwittingly instituted these perpetuating factors. That would keep us in a state of insomnia. The target of behavioral therapy is to get rid of those perpetuating factors.
因此,行为疗法的目的(如果您会认识到此图,现在这里清理了一下)处于病前状态,这些易感因素在我们的一生中都将保留,有时会出现这些易感因素,这会使我们超过失眠阈值。当发生这种情况时,即使实际的诱发因素降至失眠阈值以下,问题仍然是我们无意中建立了这些持续因素。那会使我们处于失眠状态。行为疗法的目标是摆脱那些持久的因素。
So let’s talk about the relaxation technique. Relaxation therapy is divided into two different classes. There’s Progressive Relaxation and there’s Relaxation Response. Both of these are somewhat helpful. They probably don’t work by themselves.
因此,让我们谈谈放松技巧。放松疗法分为两个不同的类别。有渐进放松,有放松反应。这两者都有所帮助。他们可能自己无法工作。
So Progressive Relaxation is the technique where one relaxes a muscle one at a time until the whole body is relaxed. The thing is they start in the face for about one to two seconds and then go down the body and repeat it for about 45 minutes. I’m telling you: if I did this I would probably fall asleep before I got to my arms; I’m just guessing.
因此,渐进式放松是一种技术,一种技术可以一次放松一块肌肉,直到整个身体放松。问题是,它们从面部开始约一到两秒钟,然后从身体向下重复约45分钟。我告诉你:如果我这样做,我可能会在入怀之前就睡着了;我只是在猜。
Another technique is the relaxation response where the patient is lying down. They close their eyes. They allow relaxation to spread throughout their entire body and they turn their thoughts to more peaceful things. So this is basically a way of just getting some anxiety-inducing thoughts out of their body. It probably doesn’t work by itself, but nonetheless, it is mentioned in the literature. So I thought you should know about it.
另一种技术是患者躺下时的放松反应。他们闭上眼睛。它们使放松散布到整个身体,并将思想转变为更和平的事物。因此,这基本上是从他们的体内摆脱一些引起焦虑的想法的一种方式。它可能无法单独运行,但是尽管如此,它在文献中已经提到。所以我想你应该知道这一点。
The next one is sleep restriction therapy. This is probably the most powerful and I would say again that this is not something that you want to do without supervision. You don’t want to do this without a physician monitoring you, but it’s an interesting situation. Now, remember we talked about how long somebody was in bed for. It’s possible that they stay in bed literally for 12 hours a day, even though they’re only sleeping six hours, and that, of course, would be asleep efficiency of 50%, so 6 divided by 12 is 50%.
下一个是睡眠限制疗法。这可能是最强大的功能,我再说一遍,这是您在没有监督的情况下不想做的事情。您不希望在没有医生监督的情况下执行此操作,但这是一种有趣的情况。现在,记得我们谈论过某人卧床多久了。即使他们只睡6个小时,他们每天也有可能每天躺在床上12个小时,而睡眠效率当然是50%,所以6除以12就是50%。
The problem is that sometimes a perpetuating factor of insomnia is that people tend to stay in bed longers, which is not good. So you might get a circadian shift with a decrease in homeostatic drive. That means just basically you don’t feel sleepy, and the more you don’t feel sleepy the more you want to try to stay in bed, so you can make up your sleep. This could be a vicious cycle.
问题是,有时失眠的一个持续原因是人们倾向于长时间卧床休息,这不好。因此,随着稳态驱动力的降低,您可能会发生昼夜节律转变。这意味着基本上您不会感到困倦,而您不感到困倦的程度就越多,您想尝试卧床休息的次数也就越多,因此您可以补足睡眠。这可能是一个恶性循环。
The purpose of sleep restriction therapy is to increase sleep drive and to consolidate sleep and sleep efficiency. So instead of having a huge denominator, which is the amount of time that you spend in bed, and a small numerator, which is the amount of sleep that you get, we want to decrease the denominator to such a small level that your sleep efficiency is big even though your total sleep time may not be big, and then slowly give back that sleep time.
睡眠限制疗法的目的是增加睡眠驱动力并巩固睡眠和睡眠效率。因此,我们希望将分母减小到一个很小的水平,以使您的睡眠效率提高,而不是拥有一个大的分母(这是您在床上度过的时间)和一个小的分子(即您的睡眠时间),即使您的总睡眠时间可能不长,也还是很大,然后慢慢地将其归还给您。
So what we do is we add up all of the fragments by looking at a sleep diary and hopefully, it’s no less than five hours of time, because if it is, it could actually be counterproductive. We count back from the target wake time. For example, let’s say you go to bed at nine o’clock at night and you get up at six, but you’re only sleeping for 5 hours during that nine-hour period though. It’s in bits and pieces.
因此,我们要做的是通过看一本睡眠日记将所有片段加起来,希望它不少于5个小时,因为如果这样的话,实际上可能适得其反。我们从目标唤醒时间开始倒数。例如,假设您晚上九点睡觉,六点钟起床,但是在这九个小时中,您只睡了5个小时。它是零零碎碎的。
So what we would do is we say okay, you slept for five hours and you want to get up at 6 o’clock in the morning. So let’s count 5 hours backwards from six o’clock in the morning, and we’ll figure out the time that you should go to sleep. Well, that’s one o’clock in the morning. So what we would say then is the patient is only allowed to go to bed at 1 o’clock in the morning. Until the sleep efficiency is greater than 85%, nothing is going to change, so every night that patient has to stay up and go to bed at 1 o’clock in the morning.
因此,我们要做的是,说好,您睡了五个小时,想早上6点起床。因此,让我们从早上六点开始倒数5个小时,然后我们便算出应该睡觉的时间。好吧,那是凌晨一点。因此,我们要说的是,患者只能在早上1点上床睡觉。在睡眠效率大于85%之前,什么都不会改变,因此患者每天晚上都必须起床并在早上1点上床睡觉。
Now one or two things will happen. Either the patient won’t be able to go to sleep and they’ll get less than five hours of sleep at six o’clock in the morning when it’s time to get up. They’re going to be really tired, which is great because that’ll help us the next night have them fall asleep more easily at one o’clock in the morning, and hopefully stay asleep until 6:00. Once that sleep efficiency gets above 85%; in other words, once they’re sleeping a solid five hours between one o’clock in the morning and six o’clock in the morning, then we’ll give a back 15 minutes now.
现在将发生一两件事。要么患者无法入睡,要么早上起床时间凌晨六点不到五个小时。他们会真的很累,这很棒,因为这将帮助我们第二天晚上让他们在早上1点更容易入睡,并希望直到6:00才能入睡。一旦睡眠效率达到85%以上;换句话说,一旦他们在凌晨1点到凌晨6点之间稳定地睡了五个小时,那么我们现在就退后15分钟。
They get to go to bed at 12:45, and if they can continue to maintain an 85% sleep efficiency, then we’ll continue to march back every week or two weeks every 15 minutes until finally where you get seven, eight hours of sleep, and their sleep efficiency is maintaining above 85%. The rule is that there is no napping.
他们在12:45上床睡觉,如果他们可以继续保持85%的睡眠效率,那么我们将继续每周或每15分钟两周前进一次,直到您获得七个,八个小时的睡眠时间睡眠,他们的睡眠效率保持在85%以上。规则是没有小睡。
Here’s an example of a sleep diary, and you can see here that we have the days of the week. They mark a line here when they go to bed, and the next morning they shade in the areas here where they actually slept. Okay, here’s an example again: the down arrow is when they go to bed; the up arrows when they wake up, but you can see here there’s significant breaks in their sleep, so this is called sleep fragmentation. This is a low sleep efficiency, and what we’d like to do is consolidate this; kind of like you defragment a computer hard drive. We want to slide all of this here toward the front end.
这是一个睡眠日记的示例,您可以在这里看到我们每周的工作日。他们上床睡觉时在这里划了一条线,第二天早晨,他们在他们实际睡觉的地方遮荫。好的,这又是一个例子:向下箭头是他们上床睡觉的时间;他们醒来时会看到向上箭头,但是您可以在此处看到他们的睡眠出现明显中断,因此这称为睡眠碎片。这是一个低睡眠效率,我们想要做的就是巩固它;有点像您对计算机硬盘驱动器进行碎片整理。我们想将所有这些滑到前端。
Say they cannot go to sleep until that time, and if they can maintain the sleep efficiency, then they get time back here. It is again graphically. So here’s the baseline of insomnia: 11 p.m. 7:00 a.m. You can see here clearly that they’re only sleeping for a certain amount of time for five hours. So what we do is we push it all the way to the front and say you are not allowed to go to sleep until this period of time, and if they maintain that sleep efficiency at 90 percent here in this case, then they get to go to bed a little bit earlier in Week Two.
假设他们要等到那个时候才能入睡,如果他们可以保持睡眠效率,那么他们就有时间回到这里。再次以图形方式显示。这是失眠的基准:晚上11点上午7:00,您可以在这里清楚地看到他们只睡了一定时间达五个小时。所以我们要做的是将其一直推到最前面,并说直到这段时间您才被允许入睡,如果他们在这种情况下将睡眠效率保持在90%,那么他们就可以入睡了。在第二周早些时候睡觉。
So the key here is to restrict the number of hours in bed, and that should be around the average total sleep time, and you really don’t want to limit it to less than 5 hours. If you do, it could be dangerous. The patient’s time in bed and out of bed is inflexible. They cannot change that; it has to be exactly that way.
因此,这里的关键是限制卧床时间,该时间应在平均总睡眠时间附近,您真的不想将其限制在5小时以内。如果这样做,可能会很危险。病人躺在床上和下床的时间不灵活。他们无法改变这一点。一定是那样的。
We try to review ways to stay awake during these times, here with they want to go to bed, but they can’t. They keep this diary and their ticket to get more sleep time is when they come back after one week and show that they’re able to stay asleep, and the titrate it based on the diary data that we get from the patient.
我们试图回顾在这段时间保持清醒的方式,这里他们想睡觉,但是他们不能。他们保留这本日记,而获得更多睡眠时间的门票是在一个星期后回来时证明自己能够保持睡眠,并根据我们从患者那里获得的日记数据进行调整。
So sleep restriction therapy: the key there is you got to monitor these patients very carefully for sleep deprivation. You got to assess what kind of a job they have and how safe is this because this is pretty serious behavioral therapy.
因此,限制睡眠疗法:关键是您必须仔细监控这些患者的睡眠不足。您必须评估他们有什么样的工作以及这有多安全,因为这是非常严重的行为疗法。
Let’s talk about cognitive therapy. Cognitive therapy is to prevent people from making a mountain out of a molehill. Basically, this is catastrophic thinking, so this is the type of patient that goes to bed and they can’t go to sleep and they say this is horrible. This is a disaster. I have a meeting tomorrow. I think this is not good for my health. I’m going to die young. I’m going to lose my job, and that type of thinking of course is not very conducive to falling asleep, right?
让我们谈谈认知疗法。认知疗法是为了防止人们有过激反应。基本上,这是灾难性的思考,所以这是上床而无法入睡的患者类型,他们说这很可怕。这是一场灾难。我明天开会。我认为这对我的健康不利。我快死了。我要丢掉工作,这种想法当然不利于入睡,对吗?
So, we need to do is we need to deconstruct that perpetuating factor of catastrophic thinking. We have to say, look, you didn’t sleep tonight, but you haven’t slept well for months and you’re still alive. You still haven’t lost your job. So it’s actually not as bad as you think. So by deconstructing that catastrophization of insomnia, hopefully we can actually get these patients to bed and forget the anxiety that they have, and forget that association of anxiety with the bedroom, so it’s multifaceted.
因此,我们需要做的是解构灾难性思维的永恒因素。我们不得不说,看,您今晚没有睡觉,但是您几个月都没有睡好,而且还活着。您仍然没有丢掉工作。因此,实际上并不像您想的那样糟糕。因此,通过消除失眠的灾难性现象,希望我们实际上可以使这些患者上床睡觉,而忘记他们所拥有的焦虑,而忘记了焦虑与卧室的联系,因此它是多方面的。
Finally, this cognitive behavioral therapy is really the whole kit and caboodle put together. In fact, you’ll see this often regarded as CBTI, and this is what psychologists do specifically. When we sleep specialists send our patients for CBTI, they’re actually very good at doing this although physicians can do it, and you don’t even have to be a physician to do this sort of stuff.
最后,这种认知行为疗法实际上是将整个套件和Caboodle放在一起的。实际上,您会看到这通常被视为CBTI,这是心理学家专门做的。当我们的睡眠专家将患者送给CBTI时,尽管医生可以做到,但他们实际上非常擅长CBTI,而且您甚至不必成为医生即可进行此类工作。
So basically cognitive behavioral therapy is a combination of everything. We’ve just talked about under the banner of Behavioral Therapy, sleep hygiene and stimulus control. So there’s education, stimulus control, sleep restriction, cognitive therapy, sleep hygiene. Basically what you’re doing here is providing your patience the tools for their future success not only to get better, but to stay better. Very few can do a good job of this, so got to do a lot of reading and figure this stuff out to not only understand it but execute on your patience. It has been proven to be effective to improve sleep quality and decrease awake time during the night.
因此,基本上,认知行为疗法是一切的结合。我们刚刚谈到了行为疗法,睡眠卫生和刺激控制的旗帜。因此,有教育,刺激控制,睡眠限制,认知疗法,睡眠卫生。基本上,您在这里所做的就是为您的耐心提供工具,以使他们将来取得成功,不仅要变得更好,而且要保持更好。很少有人能很好地做到这一点,因此需要大量阅读并弄清楚这些东西,不仅可以理解它,还可以耐心地执行。事实证明,这种方法可有效改善睡眠质量并减少夜间的清醒时间。
So cognitive-behavioral therapy is basically the summation of all of what we’ve talked about: behavioral therapy, sleep hygiene, stimulus control therapy. I know this is a quick run-through behavioral therapy. We are going to talk about medications next. This is really what people expect when they come and see their physician. What kind of medication can they give me to fall asleep a lot of times though.
因此,认知行为疗法基本上是我们所讨论的所有事物的总和:行为疗法,睡眠卫生,刺激控制疗法。我知道这是一种快速的行为疗法。接下来我们将讨论药物。这确实是人们来见医生时的期望。他们可以给我很多时间服用哪种药物。
This behavioral therapy is skip that I think that’s that’s not doing our patients a service. But let’s talk about medications in the next lecture. Thanks for joining us.
我认为这种行为疗法是跳过的,这并不是在为我们的患者提供服务。但是,在下一个讲座中,我们将讨论药物。感谢您加入我们。


Add comment