bilevel ventilation
Let me talk a little bit about non-invasive positive pressure ventilation. This is known as non-invasive positive pressure ventilation. That’s the abbreviation the other thing that we accompany this with is BiPAP.
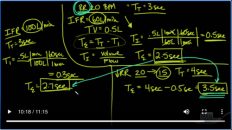
Okay, so a couple of things that you need to know in terms of setting there’s always a backup rate.
Which is just works like a backup right on a ventilator. The thing here that you’ve got to realize is that this is not an endotracheal tube going down in the patient. This is a non-invasive mask. And so you’ve got to be careful about break down on the nose. So if this is a BiPAP mask that fits over the patient’s nose, you make sure you want to have some sort of a patch or a foam or something that’s going over the nose to protect it. Okay, so you need to protect
Up the nose.
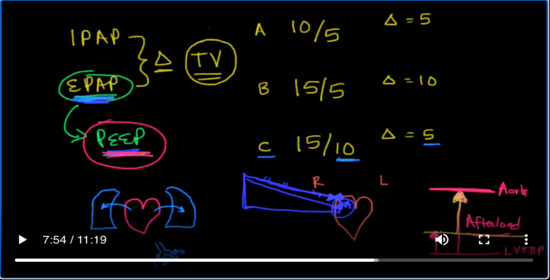
Otherwise you could get breakdown and and the nurses get really upset when the patient gets decubitus skin breakdown. They watch that like a hawk. This is no different. Okay, so you’ve got to make sure that we have got that bridge of the nose covered. Okay, but there’s two major things actually three major settings that you’re going to set on a BiPAP machine. One of them is known as the I pap.
Okay. The other one is the E pap.
And then finally, there’s the fio2 the fio2 is very similar to the fio2 that you would put into a ventilator the iPad app stands for the inspiratory.
positive airway pressure
and the E Pap of course is the expert Tori.
Okay. So these are set on the BiPAP machine just like you would set a number on a ventilator.
And these settings are typically in centimeters of water.
Okay, and they range for the iPad app anywhere between 10 to 20 and 4 e Pap, you know 5 to 10.
So let’s talk about a little bit what the definition of those things are.
The way I like to think about the I pap.
and the E pap
is this Delta? So the difference between the iPad app and the E Pap in terms of a number is going to be my driving pressure. It’s going to be the title volume that the patient is going to experience. I want you to I want you to think about this in terms of a tidal volume for this patient. So the difference between these two so let’s let’s come up with some settings here. Let’s go with 10 over 5 as it’s commonly written another one that we could do is
15 over 5. Okay. Another one that we could do is 15 over 10. Okay. So here are some examples of BiPAP and I and E paps. So here the Delta would be five here. The Delta would be 10. And again here the Delta would be 5 so in terms of driving pressure.
the
example B has the biggest driving pressure and it’s probably going to ventilate the patient the most in terms of those settings the E pap.
I want you to think about in terms of it being peep.
Okay, because basically it’s the pressure that is left at the end of exhalation. This peep can be used for a lot of different things. Okay. This can be used especially and where I like to use it is in patients with congestive heart failure. You’ve got to realize there’s a couple of things that are going on in patients with congestive heart failure. Remember, here’s the heart
and you’ve got the lungs.
Okay next to it and when the heart’s not working what’s happening is fluid is backing up into the lungs and specifically their backing up into the alveoli.
What is peep going to do in that situation or in this case CPAP what Peepaw reap app is going to do is it’s basically leaving pressure in the alveoli. And so it’s app to push that fluid out of the alveoli.
That’s really what you want to do. This. Delta is not going to be the thing that does it. It’s actually the Eep app that does it and so for instance letter C would be a better mode of BiPAP or better setting on BiPAP because it has the highest CPAP. Therefore it has the highest end expiratory pressure that’s going to be there at the end of exhalation and it’s going to push that fluid out of the alveoli. It’s gonna recruit that alveoli.
It’s going to allow that alveoli to be useful in terms of gas exchange because it’s pushing that fluid from congestive heart failure out of the alveoli back into the vasculature, even though the ventilation here is only five because of this e Pap you’re pushing that fluid out now, let me tell you something else that it’s going to do and we’ve alluded to this before remember we said that the E Pap is like Peep and what is peep do peep increases the intrathoracic pressure.
So that’s important for two reasons. Okay. It’s going to be important for the right side of the heart. It’s also going to be important for the left side of the heart. Remember that the heart sits in the intro thoracic cavity. And as a result of that when the venous return is coming back to that right atrium. Again, it’s going to elevate that and so now in congestive heart failure, this is actually going to be beneficial because instead of a lot of venous return coming back to the heart.
There’s going to be less.
Which is exactly what we want and congestive heart failure. We want less venous return coming back to the heart. And so that intrathoracic pressure that peep that Eep app is not only going to push the fluid out of the alveolus. It’s also going to raise the pressure in the right atrium and have less venous return coming back. So it actually has two usefulness has but let me tell you one other thing that it’s going to do it’s going to do something else.
If this is the pressure in the aorta.
And this is the pressure in the left ventricle. So left ventricular end diastolic pressure. Then when the ventricle contracts, it’s got to push the blood all the way up to meet the pressure and they order this is known as afterload.
What’s going to happen when you increase the peep?
When you increase the peep, the intrathoracic pressure is going to go up and because the heart sits in the intrathoracic cage, the lved p is also going to go up and as a result of that and here’s the beautiful thing about that.
your afterload produces
Okay. So this is what I love about BiPAP and patients who come into the hospital with congestive heart failure if I can get to them early enough and I can get early enough to them so I can avoid intubation. I’m going to put these patients on BiPAP. But if I put these patients on BiPAP with an E Pap of 5, I’m wasting my opportunity. Okay. I’m wasting my opportunity. These are the patients that I love to elevate the EPA.
On so I’ll Elevate the EPA up to 8 or even 10 and there’s three reasons for it. The first reason is again to review is I’m pushing the fluid out of each alveolus. That’s number one. Number two. I’m increasing the right atrial pressure. So I get less venous return which is exactly what I want in congestive heart failure. And then finally number three. I’m reducing afterload by reducing afterload in these patients. The heart doesn’t have to work as hard and therefore I
I’m actually reducing the amount of energy that the heart needs to expend, which is very important, especially in these congestive heart failure patients. The thing that you’ve got to remember however about increasing the E Pap when you increase CPAP when you increase CPAP from 5 to 10
You if you do not change the iPad app, you’re going to drop your driving pressure. So just be aware of that. If you are set on maintaining a certain title volume, you’ve got to go up on both to maintain the Delta. That’s just pure mathematics. Okay. So the one that I would like to use is 15 over 10, so let’s say I get a blood gas and the patient’s chest x-ray looks great. I’m getting rid of all of the pulmonary edema and the patient’s oxygenation is improving.
But I want to ventilate the patient more.
So, what would I do in that case? I would go up on the iPad app, but I would leave the E Pap where it is.
Okay. So this is how you manipulate these iPad Mini pain patients with BiPAP. You get a blood gas if you want to okay, so let’s just review this here get a blood gas if you want to change ventilation.
Then you need to change the Delta. If you want to improve oxygenation, then you need to change the E pap.
Okay, but realize that if you increase the Eep app and you want to keep the Delta the same then you have to increase the iPad to keep the Delta the same.
Okay, so ventilation which is CO2 and oxygenation CPAP affects oxygenation.
Changing the Delta which is number Delta is equal to the I Pap – the E Pap. So in this case, the Delta here is 5 in this case here. The Delta is 10 and this case the Delta is 5. Okay, so that’s how I would deal with patients with this. Now if a patient’s got COPD and you think there’s a little bit of auto-peep going on. I would also go ahead it for the same reasons put them on a higher EP.
App. Okay. So with that you should be able to manage just about any BiPAP ventilator.

Add comment