Asthma Diagnosis & Treatment (Video 2)
Medcram.com. Okay. Well, welcome to other medcram lecture. We were just talking about asthma in our first lecture about the causes the pathophysiology where exactly this is happening. This is happening in the small Airways, there’s many different causes for asthma. Some people just have asthma because of the air, they breathe in the other genetic makeup that they have. But there are things that can actually mimic asthma and set it off, and if you get rid of these things, you can make it better. So like things like gerd, gastroesophageal reflux disease, post nasal drip some
Some people even have a condition to associate with Samplers Triad, where they take an aspirin, or an NSAID of some sort like ibuprofen or leave. And this can cause the patients to actually get set off an asthma exacerbation. So things to look out for what we could talk about today, though, is the diagnosis in this lecture
So asthma is a clinical diagnosis, type of things that you might hear about, in patients are patients, who say, you know, when they breathe cold air, they suddenly get a tightness in their chest and it’s hard to breathe. They may we, please, maybe exercising because they’re exercising, the air that’s moving through their lungs is moving so quickly that it can’t be warmed. And so, the air inside the bronchus is is cool enough. So that it’s going to actually cause inflammation and constriction. Other things that can cause as
asthma is just an allergy to food that can cause them to get it. So these these type of symptoms of wheezing chest, tightness episodic after they do things or if they smell different types of perfume, or if they’re around someone with cigarette smoke, this should make you think of asthma. But how do we make a numeric diagnosis? We can do something called pulmonary function tests. And if you have any questions on that, please refer to our pulmonary function test lectures. The thing about pulmonary function test
That may be misleading is of course that asthma is reversible. So sometimes it’s bad, sometimes it’s good. So if you schedule a patient for pulmonary function tests and their asthmatic, you just don’t know it yet and they go in and they’re having a good day. Well, the pulmonary function tests may just come out as being normal, so then what do you do? Well, it’s also possible that it might come out to be abnormal and it may show obstruction and from our lectures, you know, that obstruction is where you have a nephew V1 divided by FEC of less than
0.7. That’s also the definition for COPD. The nice thing about COPD Ironically in that case. Is that COPD doesn’t get better so it doesn’t matter when you get there pulmonary function test, it’s always going to be less than .07, but because this has reversible Airway inflammation and obstruction, it’s possible that you could send the patient in there, having a good day and they’ve got a normal pulmonary function test. Well, if that’s the case, you do a provocative tests at that point, that provocative tests you’re provoking the small,
Ways to see whether or not they’re reactive in nature. And the name of that test is called a methacholine challenge test. So that’s a methacholine challenge.
And that’s where we have patience breathe in a concentration. Very small concentration of methacholine. Ow, you should know, choline. It’s a analog of a muscarinic Agonist and you as you recall from our first lecture, if you stimulate the smooth muscle with, choline, or acetyl, choline, or a muscarinic Agonist, you’re going to get constriction. Usually, if a normal person were to breathe in a methacholine concentration. Nothing should happen. But if they
Checked and there are ways gets smaller. That is suggestive that they have reactive Airways disease or in this case asthma and let me kind of plot for you what this looks like. So if you were to graph this and we were to plot fev1 here on the y-axis and arbitrarily set this to a hundred percent. That’s what the patient can do. And then what we do here is we do different trials.
Okay, here we do a control and of course the patient, by definition is always good to breathe that 100% of their first try. And then, what we start to do is we start to use a very small concentration, like let’s say 1 to the 16th concentration of methacholine and we keep going 1 to the 8th, one to the fourth one. Half one concentration, and we see what happens now in a normal patient you’re going.
To really have much change at all.
Okay, so this is what they would look like. This is a patient without asthma without reactive Airways disease. However in a patient with asthma, depending on if it’s very reactive or not so reactive. Let’s let’s pretend that they in this case are very reactive, you might see something like this.
Okay. And if they weren’t very reactive, let’s say they were mildly reactive. You might see something like this.
Okay, now, the lie, I didn’t draw for you at the beginning was the 80% mark because that’s the key that’s what determines when we stop this test. So clearly here in the very reactive patient, going from 1 to 16 to 1 to 8, we crossed the line at this point and so when that were to happen, we would have reached a reduction by about 20% in fev1 or more and the patient would then show reactivity. So
Positive test at that point. The next thing we would do of course, is instead of giving 124 concentration we will give them a beta Agonist like Albuterol and it would go back up this V shape. On a methacholine is suggestive and very indicative of reactive Airways disease. Same thing for this patient, we would do the same thing. Now, the purple versus the blue, the purple reacted earlier in the test meeting this patient is more reactive, the blue reacted later in the test meaning less reactive but still reactive the
So is the one who never reacted. So the purple and the blue would both be diagnosed with reactive Airways disease. And again, this is a methacholine challenge test. Okay, let’s talk about the treatment of asthma.
Okay. So since asthma is a reactive disease before we even start talking about medications, we got to start looking at what may be causing it. So I want to spend a little bit of time here because if you just skip to the medication part, you could be overlooking something that you might be able to get rid of because medicines have side effects. Especially if you could be putting this patient on a medication for a long period of time, you want to make sure that you’re not giving the medication that they don’t need.
So you need to remove causes and I alluded to this earlier, but some of the things that I would definitely look at is down comforters.
Down, pillows. So, these are down, feathers. You’re putting up right next to your nose right next to your face. You’re sleeping with it, and you’re staying for six or seven hours a night. Definitely want to consider that putting a mattress cover on pets, that sleep with you.
Okay, sometimes you’re allergic to the pets, getting them out of the bedroom, looking for other things, that might that you can control, you know, you can’t control everything. There is, there’s pollen in the air, you can’t control that but these things in your environment you can control. So looking for those sorts of things looking for post nasal drip treating that the treatment for that is intranasal. Corticosteroids looking for gastroesophageal reflux disease. This is a big one. Don’t underestimate how much gastroesophageal reflux disease.
He’s driven asthma. There is out there. The treatment for GERD is making sure the patient is elevated. When they go to sleep at night, making sure they don’t eat anything. Three hours before they go to bed, making sure they’re avoiding spicy foods. Avoiding alcohol, caffeine cigarettes, that sort of thing. So I can’t stress enough looking for the underlying cause because this is a reactive disease and we really need to make sure that we’re eliminating that. Once you’ve done that let’s talk about pharmacotherapy. Okay so everybody is good.
To get certain types of medications and the one that everyone’s going to get is a sabbah s a ba that’s a short-acting beta-2. Agonist specifically its albuterol comes in many different forms. There is also, this is an enantiomer, there’s a d and an L, or an r and s form. The other one that you will see is leave Albuterol.
Okay, there’s many different brand names for albuterol. There’s Pro are, there is a ventolin, there is xopen X, which is the brand name for leave albuterol. Everybody needs to carry one of these around with them wherever they go. And they need to be educated on that because you never know when an asthma exacerbation is going to hit. They need to make sure they’ve got a rescue inhaler with them. Now there’s always the debate metered dose inhalers versus nebulizers, there’s really no difference between these two, the
The eyes which are the metered dose inhalers are actually easier to carry around the nebulizers. You got to have power. For some people, can’t activate the mdis and so in those cases, I don’t have a problem, giving nebulizers. These are the things that people use on a as-needed basis. So, if they have an exacerbation, they can use it. It’s usually prescribed up to every four to six hours, to Puffs, that type of thing. So everybody gets one of these things, no matter how severe their asthma is. If it’s very mild, this may be enough. So if they’re only having an exacerbation,
In once or twice a week or flare up, this may be all that they need. Now if they’re having difficulties with exercise and they know exactly what it is, that flares, it up then they can take this before. They’re about to do that exercise. And that would eliminate the need for it later. It’s always better to treat before the problem comes. Then after there is a distinction made between intermittent and persistent asthma intermittence.
Is if it’s two or less times per week, okay? If that’s the case, then this is all you need. If it’s persistent. However,
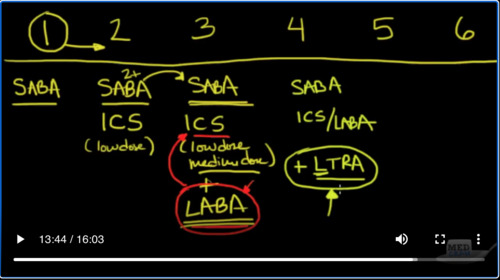
If you’re having to use, this albuterol, inhaler more than two times per week, then it’s persistent at that point. We need to go to something higher and we’ll talk about that. Okay, so let’s talk about these steps that are reported in terms of treatment from 1 being. The least severe all the way up to six, being the most severe. And as we talked about Step One is the intermittent asthma. And so the sabba or The short-acting beta-2 Agonist
Is all that’s needed. Once you have more than two exacerbations per week because of the fact that you’re having inflammation, that’s the Cornerstone there. You’re going to start the patient. Everybody gets a Sab, of course, but you’re going to add an inhaled corticosteroid and you could start this out of the low dose and go from there. So I’ll say a low dose.
When you get to step 3 if that’s not working and if you’re if the patient is still using this to 2 plus times per week then move on to the next step which would be of course keep using that seba if you have to and use that low-dose inhaled corticosteroid. So you can use low dose or medium dose.
Okay, and these inhaled corticosteroids, by the way are medications, like fluticasone, mometasone budesonide. These are all inhaled corticosteroids that come as package and many different marketing tools. You’ll see Advair, you’ll see Symbicort you’ll see dual era. These are all inhaled corticosteroids as combinations. So you use the sabbah, which is the albuterol that’s going to take care of your exacerbations and then you want to add this inhaled, corticosteroid to reduce the inflammation and so you
Either increase the dose to medium dose, or at step three. What you can do is you can add a lab, La, be a, and that’s a long-acting beta Agonist, not a short-acting, but a long-acting. Now, I want to make a point here. That’s important there long-acting beta agonists are medications. Like, sell me tirol and for Adil, okay, for model role and sell me draw these the, to long-acting Beta agonists. I want you to notice an important point. They may ask you about this and test you on a test.
During this is that the laba is always added to the inhaled. Corticosteroid, never in asthma. Will we ever start a patient on a mono therapy with a laba? A long-acting beta. Agonist first before starting the inhaled corticosteroid, they have noticed. And there there’s some literature out there that there are increased cardiac deaths. When a patient is placed on, just a long-acting beta Agonist without an inhaled corticosteroid, so you can see as we step up. The lab is always added to the inhaled corticosteroid. I think I made that.
Point. Okay. Step 4. Of course, we’re going to go back and continue the sabba.
And we’re going to probably be using an inhaled corticosteroid / laba, okay? The other thing you can adhere as an alternative. Is this leuco trying receptor antagonist? That would be medications, like, Montelukast or Zephyr. Lou cast. These are medications, like, Singulair a collate. Those are the brand names for them. And remember, we talked about before, this medicine is actually very helpful. If you know, you’re dealing with something like Sam.
Triad what you’ve got nasal, polyps and aspirin or NSAID sensitivity. These are medications that that you could add at this point. And these are basically inhibiting the leukotrienes when we get it to step 5, then we’re going up to sabes. Of course, we always have the sabbah, and the inhaled corticosteroid / lab, but these are high dose inhaled corticosteroids. So we’re using very high dose in combination with your lab is. So you’ve got a low
dose and medium dose and a high dose. Now, when you get up here too step 5, there’s another medication that I’ve alluded to that you could use. Remember, we talked about ige in the first lecture, when these immunoglobulins are high, they could be driving the reaction. There’s a medication called, oh well, Liz you mab, which is actually an antibody itself, which attacks the ige antibody. Now, this is a very expensive medication.
Don’t use it very frequently and we usually use it if nothing else is going to work, but that’s another potential thing that we can use. And then finally, when you get up to stage 6, you’re using everything that we used before. But now you’re putting the patients on oral prednisone, which we don’t like to do now. Let’s talk about side effects briefly. Sabbah these are the short-acting beta-2 agonists tachycardia? You have to watch out for a fast, heart rate, inhaled corticosteroids these are inhaled corticosteroids even though they’re being inhaled.
There are some side effects that you have to be aware of osteoporosis.
Pneumonia.
Make sure your parents are aware of this. Also, you need to rinse mouth out after use, because they can cause fungal infections on your tongue, the old militia mab. This is got a side effect of cancer of lymphoma, so you definitely want to be having a conversation with your patients in terms of risks and benefits. The risk of cancer is pretty small and you are going to use oh, militia mab if you’ve got a higher risk of death from asthma then you would from cancer. So just be aware that you
You’ve got to always weigh the risks and benefits, of course, oral prednisone increases, your risk of osteoporosis, pneumonia and fungal infections. But this is higher than inhaled corticosteroids because this has been given orally and it’s getting into your system systemically, okay? So that was a overview of asthma. The pathophysiology causes diagnosis and treatment. Thanks for joining us.

Add comment