美国医学院讲师清晰讲肺部构造及功能;心肺互动知识;自然呼吸原理、负压通气与正压通气原理及风险;正压通气与PEEP通气血液容积量设定等。
Ventilator Pearls
What we’re going to talk about today is ventilator pearls. So, you know the basics about when a patient goes on a ventilator, and what it means in terms of endotracheal tube and inflating the cuff. There are some subtleties, however, in terms of positive pressure ventilation and what happens to the lung and the heart. What is it that a ventilator does to a patient and what are the pitfalls and how can you avoid some of those pitfalls, so that’s what we’re going to talk about in this lecture.
呼吸机知识
今天我们要谈论的是呼吸机知识。因此,您了解有关患者何时使用呼吸机的基本知识,以及气管插管和充气cuff的含义。但是,在正压通气以及肺和心脏发生什么方面有一些微妙之处。呼吸机对患者的作用是什么,陷阱是什么,如何避免这些陷阱,所以我们将在本讲座中讨论。
So the first thing you should know about is the major differences between spontaneous breathing and positive pressure ventilation. That is the pressure, so what we’re going to do is we’re going to take a look at the lungs in terms of their anatomy and how this makes actually a difference.
因此,您应该了解的第一件事是自发呼吸与正压通气之间的主要区别。那就是压力,所以我们要做的就是从肺部的解剖结构以及这实际上有何不同方面来研究一下肺部。
You can see here that we’ve got the trachea, and we’ve got the right mainstem bronchus and the left mainstem bronchus, and those go to the lungs, respectively. Now those lungs are in separate areas, and they are enveloped by something called the pleural. Each pleural is separated from the other pleural, and those lungs sit in the thoracic cavity, but it’s interesting to note that the heart also sits in that thoracic cavity.
您可以在这里看到我们有气管,我们有右主干支气管和左主干支气管,它们分别进入了肺部。现在,这些肺位于不同的区域,并被称为胸膜的东西所包裹。每个胸膜与另一个胸膜是分开的,这些肺位于胸腔中,但是有趣的是心脏也位于胸腔中。
So there is a muscle here called the diaphragm, which is split into two hemidiaphragms, and when you go to take a breath in, that diaphragm contracts, which causes it to fall. Now when the diaphragm falls, that causes a negative pressure to form in the intrapleural space. That negative pressure causes the lungs to expand, and as a result of that, air moves into that negative pressure. So that’s called negative pressure ventilation, and that’s exactly what happens in spontaneous breathing.
因此,这里有一块称为隔膜的肌肉,该肌肉被分成两个隔膜,当您深呼吸时,隔膜会收缩,从而导致其跌落。现在,当隔膜下降时,会在胸膜腔内形成负压。负压会导致肺部扩张,结果是空气进入负压状态。这就是所谓的负压通气,这就是自发呼吸时发生的情况。
So spontaneous breathing just like you’re breathing right now. We actually have a negative pressure, and air from the outside is sucked into the lungs, (The key word there is ‘sucked into the lungs’) so that negative pressure is also transmitted to the heart, specifically to the right side of the heart, and that causes more blood to come to the right side of the heart. We’ll talk about that later.
因此,自发呼吸就像您现在正在呼吸一样。实际上,我们有一个负压,并且外界的空气被吸入肺部(关键词是“被吸入肺部”),这样负压也传递到了心脏,尤其是心脏的右侧,这会使更多的血液流到心脏的右侧。我们稍后再讨论。
So on inspiration, the right side of your heart actually gets more blood. So that’s what happens in the spontaneous mode of ventilation. This would occur if you’re not on a ventilator or if you’re not on positive pressure ventilation, you are just breathing normally.
因此,在呼吸时,您的心脏右侧实际上会吸收更多的血液。这就是自然通风的情况。如果您不使用呼吸机,或者如果您不使用正压通气,那只会发生正常的呼吸。
If we were to graph this Pressure versus Time and we were to start at zero, what we would see is that you would start off at your functional residual capacity (FRC), as you were to take a breath in, the pressure would go down, and then when you were to relax your lungs and let the air come back out again, the pressure would come back up to a regular baseline.
如果要绘制此压力与时间的关系图,我们将从零开始, 我们将看到的是,开始呼吸时,您将从功能残余容量(FRC)开始,然后压力下降,然后放松肺部,让空气散出再次,压力将回到正常的基准。
Now in the case of a ventilator, we have positive pressure ventilation where an endotracheal tube is going down into your lungs, and the endotracheal tube is also hooked up to a ventilator. That causes air to be pushed into the lungs. So we’re not having a negative intrapleural pressure. We’re having positive pressure and this could happen if you’re either on a ventilator or you’re on a BiPAP or a CPAP machine. In both of these cases, you’re going to see a deflection that looks like this, and then back again.
现在,对于呼吸机,我们有正压通气,其中气管导管向下进入您的肺部,并且气管导管也与呼吸机挂钩。这导致空气被推入肺部。因此,我们的胸膜内压力不为负。我们的压力很大,如果您是在呼吸机上,或者是在BiPAP或CPAP机器上,则可能会发生这种情况。在这两种情况下,您都会看到这样的偏转,然后再次返回。
So here is the key that you must understand between negative pressure and positive pressure ventilation: the intrapleural space goes through a completely different type of pressure change depending on whether you’re on negative pressure ventilation or positive pressure ventilation, and that has significant consequences, which we’ll talk about.
因此,这是您在负压和正压通气之间必须理解的关键:胸膜腔空间会经历完全不同的压力变化类型,具体取决于您使用的是负压通气还是正压通气,这会产生重大后果,我们将讨论。
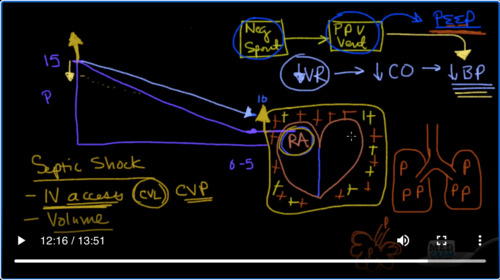
So here are some of the consequences that can happen. Here we have our heart, and of course, we know that all venous blood comes back to the right atrium. As we said, this heart sits in this cavity called the intrathoracic cavity, which is generally negative, and that helps out because as you recall all blood goes back to the right atrium.
因此,这里有可能发生的一些后果。在这里,我们有我们的心脏,当然,我们知道所有静脉血都回到右心房。正如我们所说,心脏位于这个称为胸腔的腔中,通常是阴性的,这会有所帮助,因为当您回想起所有血液都流回右心房时。
So here we have again Pressure, and pressure is starting out at around 15 and coming up at around zero to 5, which is right about here. So here is the barometric pressure, or here’s the pressure in the right atrium, which is about 0 to 5. It’s sitting in the negative intrathoracic space and the venous return is quite nicely sliding down the slide.
所以在这里我们又有压力,压力从15左右开始,从零到5上升到正好在这里。因此,这里是大气压力,或者这是右心房中的压力,大约为0到5。它位于胸腔内负空间,静脉回流在滑道上顺滑滑动。
Now when you go from negative pressure ventilation, or spontaneous ventilation, to going on a ventilator, which is positive pressure ventilation when you intubate somebody, or put them on BiPAP or put them on CPAP, you’re going from this box over to this box. Then since this is now positive pressure ventilation, it’s going to be transmitted. That positive pressure is now going to be transmitted to the right atrium. So instead of the right atrium being at zero to five now, maybe it’s going to be up to 10, and as a result of that, this venous flow, or this venous return, is now going to be coming back to a chamber that is higher in pressure. As a result of that, there is less flow, so venous return is reduced when you go from negative pressure to positive pressure ventilation.
现在,当您从负压通气或自发通气转到呼吸机上时,这是当您向某人插管或将其置于BiPAP或CPAP上时即为正压通气,您将从此盒子转到此盒子。然后,由于现在这是正压通风,因此将被传输。这种正压力现在将传递到右心房。因此,现在的右心房可能不再是零到五个,而是可能会增加到十个,因此,这种静脉流或这种静脉回流现在将回到腔室中。压力更高。结果,流量减少了,因此当您从负压通气转为正压通气时,静脉回流会减少。
Since the heart can only pump what it’s given, this decrease in venous return is going to also drop the cardiac output, which is going to lead to a drop in blood pressure. That’s the key there that I want to emphasize to you: when you take somebody who is already maybe a little volume-depleted, or is in septic shock and is doing worse and you’re going to intubate, you’re going to take them from negative pressure ventilation to positive pressure ventilation, and you’ve got to be careful with a drop in blood pressure. That’s very very important.
由于心脏只能泵送所给予的能量,因此静脉回流的减少也将使心输出量下降,从而导致血压下降。这就是我要向您强调的关键:当您带走的某个人的身体可能已经衰竭,或者正在败血性休克的情况下变得更糟,并且您将要插管时,您将把他们带走从负压通气到正压通气,并且必须注意降低血压。这是非常非常重要的。
In terms of a real-world example of this, how many times do we see patients that come in with septic shock and their venous return is already a little bit on the limited side. So it’s going to be less. So that’s going to also decrease this slope of getting fluid back to the right atrium. They are sick, their lactic acid level is high. They look ill-looking and you’re looking at them, you’re saying you’ve got to intubate, and already let’s say their blood pressures like 90 over 60 or something low.
就现实的例子而言,在有限的方面,我们已经看到多少次出现败血性休克而静脉回流的患者。因此它将更少。因此,这也将减少使流体返回右心房的这种斜率。他们生病了,他们的乳酸水平很高。他们看起来不舒服,而您正在看他们,是说您必须插管,已经说出他们的血压超过90或90或更低。
You know in the septic shock patients, these are the ones who are already volume-depleted. And if you go ahead and intubate them and put them on positive pressure ventilation, you know that their blood pressure is just going to krump, you need to make sure they’ve got good IV access.
您知道在败血性休克患者中,这些患者的血容量已经耗尽。而且,如果继续进行气管插管并进行正压通气,您会知道他们的血压将krump,则需要确保他们的静脉输液良好。
Okay need to have good IV access; think about even doing a central venous line and give them volume because what that volume will do is it will push the pressure up and compensate for the fact that this is already been pushed up as well when you’re about to intubate them.
好的,需要有良好的静脉通路。考虑甚至做一条中心静脉线,并给他们足够的体液(VOLUME),因为体液(VOLUME)会增加压力,并补偿当您要为它们插管时已经被向上推动的事实。
So I would rather have the venous pressure up before I increased intrathoracic pressure because that way I’m not going to get as much of a drop in venous return, which will correlate with a drop in cardiac output, which will correlate with a drop in blood pressure.
因此,我宁愿先增加静脉压力,然后再增加胸腔内压力,因为那样一来,我不会获得太多的静脉回流下降,而这与心输出量的下降有关,而心输出量的下降与血压下降有关。
Also, the nice thing about getting a central line in these patients is that remember with a CVL (central venous line) you can measure the central venous pressure. Getting that central venous pressure up in the eight, nine, ten, eleven, twelve region is going to be key especially in your septic shock patients. That way you can actually measure what this right atrial pressure is going to be. That’s important to get a central line in these patients where you have some time. Sometimes you don’t have time, you just have to intubate, but just be aware that if you are and you’ve got IV access, which usually does that, you need to give lots of volume.
同样,在这些患者中获得中心线的好处是,请记住,使用CVL(中心静脉线)可以测量中心静脉压。在八个,九个,十个,十一个,十二个区域中增加中心静脉压力将是关键,尤其是在您的败血性休克患者中。这样,您就可以实际测量出正确的心房压力。这对于在您有时间的这些患者中占据中心位置很重要。有时您没有时间,只需要插管即可,但要注意,如果您已经并且可以进行IV接入(通常这样做),则需要提供大量的体液(volume)。
Let’s just take a step back just a bit. We talked about going from negative or spontaneous ventilation to positive pressure ventilation. The next step that you can go in this direction is actually adding on PEEP. What’s Peep? Peep stands for positive end-expiratory pressure; the key there is end-expiratory. So what does that mean? You now know that we are putting into the lungs a certain amount of volume, and at the end of that exhalation, volume is going to go in. Okay, and then volume is going to come back out, and at the end of that exhalation, if we decide to leave a certain amount of volume of air in the lungs, we can do that, and by doing that there’s a certain amount of pressure that’s left in the lungs.
让我们退后一步。我们讨论了从负压或自发通气转为正压通气。您可以朝这个方向迈出的下一步实际上是在PEEP上添加。偷看什么?窥视代表呼气末正压;关键是呼气末。那是什么意思呢?您现在知道我们正在向肺部注入一定量的气体,并且在呼气结束时,气体会进入。好吧,然后,在呼气结束时,气体将会出来。 如果我们决定在肺中保留一定量的空气,我们可以做到这一点,并且这样做可以在肺中留下一定量的压力。
Now that pressure is usually there to make sure to keep the alveoli open. So there are these air sacs at the very terminal end of the lungs, and by applying pressure to it, it’s going to keep these alveoli open with the help of surfactant.
现在通常存在压力,以确保保持肺泡开放。因此,在肺的最末端有这些气囊,通过对其施加压力,可以在表面活性剂的帮助下保持这些肺泡开放。
So keeping the alveoli open is very important in terms of oxygenation. Sometimes you’ll see that especially in patients with, for instance, congestive heart failure, exacerbations, or ARDS, that you’ll see that the PEEP is elevated in these patients, and the rationale for that is: on the end of exhalation, don’t let all of the air out because that will cause collapse of these alveoli, which have been recruited to give you good gas exchange.
因此,就氧合而言,保持肺泡开放非常重要。有时,您会发现特别是在患有充血性心力衰竭,急性发作或ARDS的患者中,这些患者的PEEP升高,其原因是:在呼气结束时,不要让所有的空气散出,因为那样会导致这些肺泡的塌陷,这些肺泡被募集来为您提供良好的气体交换。
People set PEEP usually like to 5, but you can set PEEP to 10 12 13. Sometimes you have to go pretty high to get oxygenation up. While that PEEP is going to be transmitted to the bronchioles, it’s gonna be transmitted to the respiratory bronchioles and finally to the alveolus as well, because that pressure is left in the lungs and that pressure is just going to get added to this intrathoracic pleural space.
人们通常将PEEP设置为5,但您可以将PEEP设置为10 12 13。 PEEP会传播到细支气管,但也会传播到呼吸性细支气管,最后也传播到肺泡,因为这种压力留在肺中,而这种压力只会增加到胸腔内胸膜腔。
That intrathoracic pleural space is going to go from negative to positive to even more positive. So just as going from negative pressure ventilation to positive pressure ventilation caused an increase in the intrathoracic pressure, going from regular positive pressure ventilation to high PEEP, or increased PEEP ventilation, is going to do the same even more, so the higher you increase that PEEP, the likelihood or chance you have of causing a decrease in venous return, which correlates to a decrease in cardiac output, which finally corresponds to a decrease in blood pressure.
胸腔内胸膜空间将从阴性变为阳性,甚至更阳性。因此,就像从负压通气到正压通气导致胸腔内压力增加一样,从常规正压通气到高PEEP或增加PEEP通气,这样做的效果甚至更多,因此,您将其提高得越高PEEP,您引起静脉回流下降的可能性或机会,与静脉血流减少有关,心跳血流减少最终与血压下降有关。
So when I’m at the ventilator, and I’m ventilating a patient, and I’m having difficulty with oxygenation, I’m going to go ahead and increase the PEEP, knowing full well that I’m going to recycle that blood pressure after I do it to make sure that I haven’t crossed the line and cause the blood pressure to drop because of drop in the venous return.
因此,当我在呼吸机上呼吸时,我在给患者通气时,我遇到充氧困难,我将继续提高PEEP,并充分了解自己将回收血液这样做后,请确保血压没有过界,并由于静脉回流的下降而导致血压下降。
It’s really good with I’ve got an arterial line so I can get real-world data back right away. It’s also helpful to know that when I’m going to increase the PEEP on a patient because of oxygenation, I may have to increase the volume to overcome that intrathoracic pressure and that barrier to venous return. Okay, so that’s positive end-expiratory pressure. And so this is all a continuum: negative to positive, to even more positive with positive end-expiratory pressure.
我有一条动脉线,这真的很好,这样我就可以立即获得真实的数据。知道当我因氧合而增加患者的PEEP时,可能还需要增加容量以克服胸腔内压力和静脉回流障碍。好的,这是呼气末正压。因此,这都是一个连续的过程:从负到正,在呼气末正压增加时甚至更大。

Add comment