Update 85: Dexamethasone and Key Questions to Ask in the Hospital (Part 2 of 2)
本文由‘中国推动’学者、济南大学生命科学学院生物技术专业任紫豪同学编辑整理。
MedCram.com
Welcome to another MedCram COVID-19 update. This is part 2 of what questions you want to ask if you or a loved one is in the hospital with COVID-19. We’re going to talk a little bit about testing and we’ll do that in another video. But let’s just look briefly at what’s going on here with total daily cases in the United States. You can see here that it’s for the most part leveling off.
But the number of deaths continue to go down which is interesting. And it has led some to speculate that perhaps the virus is getting weaker, of course could also mean that we are just getting better at treating patients. If we look at the seven day moving average, you’ll see definitely that there is a decrease in the daily deaths. Look at the three day moving average, we can see there is a weekend variation there.
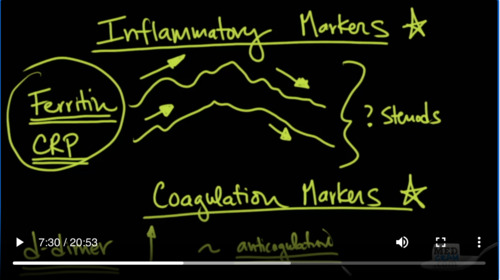
So that brings for the United States the coronavirus cases 2 over 2 million. So that brings up the question: what happens if you or a loved one in the hospital being treated with COVID-19? What are the right kind of questions to ask kind of treatment should you be on. Let’s continue on that topic. Also a couple of lab tests that you may want to talk to your doctor about. They have inflammatory markers and coagulation markers.
So let’s talk about inflammatory markers first. So ferritin does contain iron in it. And there was a discussion that occurred a couple of months ago that because the ferritin levels were high, they thought will perhaps there is a problem with iron and the hemoglobin. In fact, ferritin is something called an acute phase reactants meeting that any kind of infection any kind of inflammatory situation in the body is going to cause an increase in ferritin. So we can actually track this and as we track it we can see that as the patient is starting to recover from COVID-19, we will start to see these inflammatory markers start to descend. And if they are getting worse, we’ll see it increase.
Another one that we’ll see is C-reactive protein, same similar course though on a different scale. The numbers involved with ferritin will be in the hundreds to thousands where CRP will be in the tens. And so this is one way of telling which direction is my loved one going. Are they getting better? Are they getting worse?
Coagulation marker, something called a D-dimer. So a D-dimer is a byproduct of coagulation and breakdown in the systemic vasculature. And so if we see a lot of D-dimer if that is going up and you’ll see these usually in the tens I’ve seen as high as 30 depending on the scale. Sometimes it can be undetectable. And that’s usually where we want it to be a low D-dimer is a good place to be. Again, if we start to see it go up, we start to think of excessive coagulation and blood clots. And as we discovered COVID-19 does have a predilection to causing a lot of blood clots. And so one of things that you can do with that is consider anticoagulation.
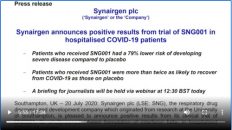
What can we do in terms of inflammatory markers? Well, the question is whether or not we ought to be giving steroids. And of course the big news today on June 16 is the release of data from the recovery trial which is looking at a number of medications. But this one particularly looking at Dexamethasone. Now Dexamethasone is a pretty inexpensive steroid that’s been around for some period of time to can be given both orally and intravenously. So in this trial, they took patients with Dexamethasone given randomly and compare them to standard of care. And they looked at several different categories.
First of all, there was 2104 patients in the Dexamethasone group, and there was 4321 patients that were in the standard of Care Group and they looked at three different categories. They looked at those patients that were not on oxygen at all. They looked at those patients that were just on oxygen and they looked at those patients that were on the ventilator. Now when they looked at those patients who got standard of care and they were not on oxygen they did not require oxygen, these patients had a 13% mortality. Those that were just on oxygen they had a 25% mortality. And those that were on the ventilator had a 41% mortality.
Now when they looked at these patients with Dexamethasone and these patients received six milligrams once a day. In one dose it was either given orally PO or intravenously IV. This is what the results were. In those not receiving any oxygen therapy that the mortality rate was 16% and that numerically is higher than 13% than in fact when they looked at it statistically, there was no statistically significant difference.
Now when they looked at those that were just on oxygen, this would be like a nasal cannula or something like that maybe a face mask. These patients had a mortality rate of 20% which was actually in comparison to 25%. It was a reduction of 20%. So there was a reduction of 20% mortality and that was statistically significant at a P-value equaling 0.0021.
And so because the mortality rate dropped by 5% that’s what we call an absolute risk reduction of 5%. If you take the reciprocal of that, the number that you get is 20. And so the number needed to treat here with Dexamethasone in this category would be equal to about 20. But the effects were even bigger in those patients on ventilators because there instead of having a 41% mortality, those on the ventilator that receive Dexamethasone had only a 27% mortality, and that’s a relative risk reduction of about 35%.
And as you can see, that’s an absolute risk reduction from 41 down to 27 of 14% which converts to a number needed to treat of about eight patients. Now just to give you a sense, Remdesivir is about 30 in terms of the number needed to treat. And so you can see here very clearly that up to this point in our battle against COVID-19 for those patients on the ventilator or on oxygen therapy, there really is nothing that comes close to what we’ve just discovered here with Dexamethasone. The fact that it’s also a pretty inexpensive medication has led Martin Landry the Oxford University Professor that’s co-leading the trial to say, quote it’s going to be very hard for any drug really to replace this. Given that for less than $63.26, you can treat eight patients and save a life.
Another good question to ask is what are the inflammatory markers? What’s the D-dimer doing? Is it going up or down? And are you starting full dose anticoagulation? Now, they may decide not to do it. There’s complications both ways. If you don’t start it, you could get blood clots. If you do start it, you could have complications with bleeding. And they can be severe bleeding into your muscles, can cause compartment syndrome bleeding into your retroperitoneal space. You can lose a lot of blood and need blood transfusions and have problems with that. So there has to be an individual choice made between the patient and the physician looking at all of these factors.
And of course everybody wants to make sure that their loved one or themselves are getting the best and latest treatment. So let’s talk about that as of mid June to late June here what is current in terms of treating COVID-19. So Remdesivir is probably one of the highest levels of evidence that we have right now. It is FDA approved. It is based on a randomized placebo-controlled trial that was stopped early at an interim checkpoint because endpoints were made. So Remdesivir is an IV medication. It cannot be given orally. Generally speaking, we want to give this as early in the course as possible because the mechanism of Remdesivir is to stop viral production or reproduction as you recall when the RNA dependent RNA polymerase is trying to make more RNA particles, Remdesivir steps in and basically shuts that down.
So one of the things that you should know about Remdesivir is if you are not intubated, the course is five days. And if you are intubated, the course is generally 10 days. Some of the exclusions, if there is significant renal problems, then we are not going to be giving Remdesivir, because it reflects and needs kidney functioning properly in that situation.
The other thing is if you have elevated liver function tests like AST and ALT, that is another reason that we would have to stop Remdesivir. So what has Remdesivir done is basically sped up the recovery process and we also believe that it improves mortality, but the studies were not complete on that.
The next one is Tocilizumab. And as you may know this is an anti il-6. Now il-6 is an interleukin. It is involved in revving up the inflammatory response against coronavirus COVID-19, and it can also cause cytokine storm. So generally speaking, this is given like x1, it can be given again later in the course. The big thing to remember about this is that you don’t want to give it if there is a super infection. By that, I mean, yes, we know that there is an infection of COVID-19 SARS-CoV-2, but if there’s also a superimposed bacterial pneumonia, like staff strep or some other bacterial pneumonia in the body, that’s making the patient sick.
Remember this is going to hamstring the immune system and you don’t want to make that worse if there is a super infection. So that’s a contraindication to giving Tocilizumab. So we’ve talked about Remdesivir. We’ve talked about Tocilizumab. Pretty good data on this. This is FDA approved for rheumatoid arthritis and other autoimmune conditions. The last one is convalescent plasma. This is still under research. So the only way you can get this is from the blood bank first of all and the patient needs to sign a consent form so that they understand that they’re going to be in a study. And you need to get a Type and Screen.
What is the Type and Screen? The Type and Screen is to tell you what type of blood you have, because based on the type of blood you have to get different types of convalescent plasma from different donors that are compatible. And you also need to make sure that the plasma doesn’t have antibodies in it that will react against your blood. The availability is the big rate-limiting step with convalescent plasma and that is related to the kind of blood bank that you have working with your hospital. Some hospitals have their own kind of Blood Bank situation, other hospitals depend on the county to contract with a provider of blood products that might be something like live stream or the American Red Cross. And so you’re going to be dependent on those for getting the correct plasma if that’s what’s necessary.
And generally speaking, we will start convalescent plasma if the patient is still getting worse despite treatment up above here with either Remdesivir and/or Tocilizumab. The other thing I would mention about Tocilizumab is it’s generally given if the patient’s ferritin levels are above 500 as a show that there is a significant inflammatory process going on. So it’s very good to ask about these things as well.
What about other treatments? Treatments that we don’t have a lot of evidence for, but it’s not really harmful either. So number one, you can ask are you giving zinc? So zinc is an oral preparation, give zinc sulfate. We’re doing that at our hospital is very little information that this is going to be detrimental to the patient’s health and it may actually be beneficial. So we’re going to do it. Some other things that may work in this situation, but we don’t have randomized placebo-controlled trial data on vitamin C. So sometimes we give that IV or sometimes we give it orally.
Number three vitamin D, there’s been a lot of talk recently also here at MedCram about vitamin D and its benefits. We don’t know if it helps in COVID-19, but we sure know that it’s associated with acute lung disease, acute lung viral infections, chest infections and supplementing that may prevent that from happening. So we also give vitamin D. And as we talked about in the past, we also can give N-acetyl cysteine, you can give that intravenously or orally, again all of these things have very low side effect profile. Again, this is going to be a little bit more of a personal decision and also discussion between them and you.
Finally, there’s probably going to be a discussion that you’re going to have regarding something called DNR status. Let me be clear that this is a discussion that we really always have to have regardless of whether or not they’re just a little bit sick. We have to have a discussion about if they can’t make medical decisions who are going to make medical decisions in their place. We believe that the patient should be able to make decisions first off. And also if they can, they should be able to decide who gets to make those decisions and what are the nature of those decisions.
And so what does a DNR status mean? It really talks about limitations of treatments and I know this sounds kind of odd. Why would you ever want to limit treatment options? Well, it’s because of the nature of the interventions that we do in medicine. Sometimes the interventions that we do in medicine are very non-invasive. Like IV fluids may be drawing some blood flipping you over on your belly for instance. All of these seem pretty innocuous. However, there are some procedures that we do that can be very invasive, for instance putting a tube down into your lungs where you can’t talk and you’re hooked up to a ventilator and you’re not really able to tell us exactly what you want.
Also, what about chest compressions? where we push on your chest into you about 2 inches so that we can get your heart to pump blood around. Sometimes we can break ribs with that. That’s a fairly invasive procedure. How about hooking up pads to your chest and putting 200 joules of electricity through your chest to jumpstart your heart, again very very painful. And so the question is should we be doing those things? We certainly want to get your permission and because of the very nature of the situations that invite us to have to do these things. We can’t always call and ask for permission at that time without compromising the health of the patient. So we need to know these things in advance. It’s not like in the movies where we do chest compressions and we shocked and almost 99% of the time the patient comes back. So let me explain a little bit about what the decisions are that you’re going to make.
The biggest thing that you’re going to have to talk about is intubation. Intubation is essentially where you have the trachea and the lungs and we put a tube down into your mouth past your tongue past your vocal cords and into your trachea. And we inflate a balloon around it, so that air can’t escape and we ventilate your lungs with this endotracheal tube. Usually at this point you’re sedated, so you don’t feel this, can’t talk. And generally speaking, you’re not going to be able to drink or eat.
Now that doesn’t mean that you won’t get nutrition. You could get that through a tube going down the same area, but this time into the stomach. Intubation can last up to two weeks and if that continues and you still need to be on the ventilator, it may lead to something called a tracheostomy not a 100% of the time but just want you to be aware of that. This is a situation where if you can’t breathe you’re hooked up to a ventilator and that is a type of life support. Generally, we hope that it’s a bridge to recovery. But in several situations where patients lungs are not very good, it may be a situation where they’re probably not going to be able to get off the ventilator in the near future. And that discussion needs to happen between the patient and the healthcare provider.
The next discussion you’re going to have is about CPR, that’s chest compressions. That’s where we actually press on the ribs and pump the heart, so that blood can circulate around and you can continue perfusion of the blood to the vibal tissues. I can just tell you that generally speaking CPR is what we do at the very end when nothing else is working. So we use effective treatments like IV fluids like medications like proning maybe even the ventilator. And if all of that fails and the heart stops, despite all of that work, doing chest compressions on the heart is rarely ever going to be fruitful in terms of providing life to come back.
In-hospital mortality for CPR is very very high and we can never call you before we need to do this because we do it immediately as soon as it is noticed on the Telemetry monitor that the patient no longer has a heartbeat. We run in there literally and start doing chest compressions for 2 minutes and we give medications to try to restart the heart and in the process we can break ribs. The default is that we will do it unless you tell us not to do it. If you tell us that you want to have CPR done, then the patient will not be able to die without having CPR done.
The last thing I want to talk about and I know this is a long video but I wanted to get this in is something called Comfort Care, whereas before here with intubation CPR, generally speaking, they’re going to continue acute care. They’re going to continue to give medications antibiotics things of that nature to fight actively the COVID-19 infection. If certain things happen, then it will take those things off the list in terms of doing them. Because they’re very invasive and perhaps they’re not going to offer the help that is beneficial over the risk of invasiveness. Here however, when we’re talking about comfort care, we’re going to focus our attention in making sure the patient is comfortable. Now while we do try to make sure that the patient is comfortable here in all the other circumstances. There’s always a problem when we try to make patients comfortable because the medicines that we use can also drop blood pressure heart rate oxygen things of that nature also mental status.
Here, with comfort care. We are giving those medications and we don’t really care if the blood pressure goes down. We don’t care if the oxygen goes down because our focus here is uncomfort. And we realize of course that there’s a double-edged sword here. There is another unintended consequence of giving morphine Ativan things of that nature and that it will potentially hasten death, but that’s not the reason why we’re doing it. We’re doing it here because we are trying to make the patient comfortable.
And if the patient is comfortable then we don’t need to give anymore that medication. And this is sometimes an option that we see some family members going for especially when someone has been suffering for a long period of time. They’re not getting better or we start to see that things are starting to unravel very very quickly and we don’t need to give those medications anymore that’s causing discomfort. We’re switching to a more palliative type of care and that is a decision that a patient can give and families know what their loved ones might want.
So of course looking at all of these if intubation is wanted in the case of respiratory failure, if CPR is wanted in the case of cardiac arrest and you don’t want comfort care but you want the patient to be comfortable but everything else done. That term is known as full code. That means everything is going to be done for that patient regardless of how effective that intervention might be or how invasive it might be or how many ribs you might break in other words in that situation.
If you or a loved one God forbid are in a situation where you have COVID-19 and you need to know more information. I hope this video has been helpful. If you know somebody who knows somebody maybe you can forward this information to them so they can make better decisions and understand better what’s happening to their loved one in the hospital. Thanks for joining us.


Add comment