Update 82: Racial Disparities with COVID-19 & Vitamin D
本文由‘中国推动’学者、济南大学生命科学学院生物技术专业任紫豪同学编辑整理。
Welcome to another medcram covid-19 update. I wanted to show you some interesting aspects under the critical Trends tab up here in the upper right-hand corner. And this one I found interesting have countries flatten the curve you can see here is a nice diagram of the confirm new cases in each of these countries, but they’re further delineate. Adhere in scaled graphs. You can see here Brazil United States.
On the right we can see Mexico and India and exactly what’s happened here up until early June you can see here that United Kingdom has nicely Flats into the curve. Whereas in Chile. It’s on the other side where things are actually escalating we can see that here also in Russia, they’ve been able to at least delay or hold off on further increases in the number of confirmed new cases. Canada’s also done a nice job of leveling them off. Whereas here in Pakistan things seem to be
Rating you can click on this button to view all of them interesting data and trends that you can see here under critical Trends on the Johns Hopkins site. And of course will include that link in the description below and if we go to our friends over at worldometer, we can also see another way of keeping track of these numbers here. You can see daily new cases for the world is actually up. Of course, there’s different hotspots and cooling off spots around the world and you
Can see the number of daily deaths is slowly decreasing may be leveling off here in late May early June and also let’s not forget covid – trials dot-org is a great website that we find that has a lot of interaction in terms of treatment and where different trials are actually being held around the world. It’s listed by country by treatment and then different areas where you can actually follow the studies and trials with links.
Wanted to talk about some risk factors for covid-19. This article just came out yesterday. This is actually the 9th of June and the article is titled diabetes may present greatest risk to covid-19 patients when newly diagnosed and this is basically data that has come out of China which links mortality from covid-19 to blood sugar levels.
And they also compared this to their humor globin A1C as you can see it on here. Now. This is kind of a running average. If you will of the amount of blood sugar in your body for the last two to three months because we can actually measure how much glycated hemoglobin is around in your blood which tells us how high your blood sugar levels have been for the last two to three months what they’re noticing here in this study and we’ll get to it is that those patients with relatively low hemoglobin a1cs in other words. They’ve been
Under pretty good control for some period of time come in with elevated blood sugar levels so acutely elevated because it hadn’t been that way for some time. These are the ones that are particularly at risk for mortality with covid-19. Now I want you to be aware for those of you who are in the United States the measurements of glucose here in this article are a little bit different there in millimoles per liter instead of milligrams per deciliter. And the way I remember that is that ten Milli moles per liter is
is about a hundred and eighty milligrams per deciliter and they say in this article from a Dwyer news.com that the size of risk increase was linked specifically to raised fasting glucose and that there was a ten point four fold risk increase in the subgroup of patients with a fasting glucose of 7.0 millimoles per liter, which is about a hundred and twenty six milligrams per deciliter, but a hemoglobin A1c below 6.5%
Set in other words an acute rise in blood sugar, but a hemoglobin A1c. That was normal. So with that you got a ten point four fold risk in covid-19. However, people who had hyperglycemia below that threshold and those with established diabetes for some period of time had a significant increase mortality, but it wasn’t as high as ten point four and this group it was only three point two nine and four point six three
Respectively now there was some other adjustments for blood pressure medication diabetes medication use of corticosteroids. And this caused the authors to say that it could be speculated that covid-19 patients with known diabetes using glucose lowering drugs to control blood sugar might have a protective effect on the death risk.
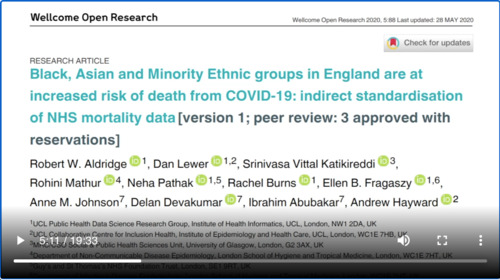
So interesting, this is a retrospective study. And so we can only say that there was an association of elevated blood sugar with increased death. We don’t know if it’s causation because there could be confounders. I wanted to switch gears and actually highlight this welcome open research article that was submitted late last month and I thought it was an interesting article because of the question of race and mortality now, there’s been some attention turned to that in the United.
States because of the published discrepancies between mortality in different racial groups and part of the explanation of that has been directed to the ability for healthcare access. So my attention was directed to this article which has not been completely peer-reviewed as you can see here. It says version one peer review three approved with reservations. And the reason why this was an interesting article is because
It’s looking at race disparity in the United Kingdom, which has a National Health Service for all and to the degree that this allows for open access to Healthcare in that country regardless of racial ethnicity. It would be interesting to see the results of that. So, let’s take a look.
So the background here is that International and UK data suggests that black Asian and minority ethnic groups are at increased risk for infection and death from covid-19. We aim to explore the risk of death and minority ethnic groups in England using data reported by the NHS England. So how do they do that? Let’s take a look at their methods. Nice thing about the NHS of course is that there’s easily able to get data and say look that deaths from the 1st of March up until the 21st of April of this year.
Here and they standardize the data looking at the entire population of England to produce ethnic-specific standardized mortality ratios or smrs for adjusted age and geographical region. And so the data here shows that the largest total number of deaths in minority ethnic groups were Indian and black Caribbean and that when they adjusted for region, they found a lower risk of death for White Irish and for white British ethnic groups, but rather an increased risk of death for
Black African black Caribbean Pakistani Bangladeshi and Indian minority ethnic groups and the way you read these is you look at the number initially. It will tell you what the risk of death is. And if it’s below one, then that would imply that there is a protective effect and if it is above one like it is here in this case 2.21 that would be an increased risk of death and of course to find out whether or not it’s statistically significant. They have something called the 95% confidence interval and
generally speaking if that confidence interval does not include the number 1 then it is statistically significant so you can see here because the range for white British ethnic groups does not include the number one. It goes from .86 to 0.89. Then it is statistically significantly different than a ratio of one here the risk for death in Black Africans is 3.24 and you so you can see here that is
Above one and does not include one in that range. So that again is also statistically significant for black Caribbean. Once again, it’s above one and one is not included in the range and so forth our analysis adds to the evidence that be AME or black Asian minority ethnic people are at increased risk of death from covid-19. Even after adjusting for geographical region. We believe that there is an urgent need to take action to reduce the risk of death for be AME groups and better understand why some ethnic groups experience.
Ian’s greater risk actions that are likely to reduce these inequalities include ensuring adequate income protection so that low paid and zero-hour contract workers can afford to follow social distancing recommendations reducing occupational risk such as ensuring adequate personal protective equipment and reducing barriers in accessing health care and providing culturally and linguistically appropriate Public Health Communications. And of course, I think this is all reasonable the part that’s interesting to me. Is that urgent?
Need to better understand why some ethnic groups experience a greater risk, and I think there’s some interesting data that is instructive on that.
And it kind of takes us back to what we’ve been talking about here in the last couple of months and specifically with vitamin D. I don’t think that vitamin D explains a hundred percent of the discrepancy, but I think there is a place at the table for talking about vitamin D deficiency, especially given some of the data that we’ve got on this I think this paper is pretty good in terms of this discussion because it was published four years ago. Well before covid-19 pandemic even has a word pandemic in the title, and the
Love this article is vitamin D deficiency in Europe. So it’s looking at the very same people in terms of population of the UK Europe etcetera. So, let’s see what they found in this article.
So the purpose of this study was to apply something called the vitamin D standardization program or the VSP protocols to serum vitamin D data from representative childhood / teenage and/or adult older adult European populations, representing a sizable geographical footprint to better quantify the prevalence of vitamin D deficiency in Europe. Again, this was published in 2016. So this is relatively recent and so they did that they took the VSP protocols.
They applied the 14 different population studies and they looked at serum 25 hydroxy vitamin D. So this is vitamin D in the body after gets hydroxylated at the 25 position in the liver. But just before it gets activated to its active form by hydroxylation at the one position in the kidney. So looked at that in 11 studies and complete analysis of all samples from three studies that had not been previously measured by using certified liquid chromatography tandem Mass spectrometry.
Tree and bio Bank syrup. These data were combined with standardized serum 25 hydroxy vitamin D data from for previously standardized studies for a total n number of over 55,000 patients prevalence estimates of vitamin D deficiency were generated on the basis of standardized 25 hydroxy vitamin D data, so they looked at this and what they found was that are respective of age irrespective of ethnic mix
Of latitude of study population. It showed that 13% of the 55,000 plus European individuals had serum 25 hydroxy vitamin D concentrations less than 30 Nano moles per liter. That’s the pretty low-level cut off. There’s some data that might indicate that you really want to get that level above 50 but taking a very conservative level of 30 nanomoles per liter pretty low here and a
nificant amount that showed deficiency 13% and realize that that 13% got higher in the winter time up to 17.7% and dwindled down to eight point three percent in the summer months from April to November. If we go with the more robust level of 15 any moles per liter, then the estimate the prevalence was a whopping 40 percent of subjects in the study in Europe could be considered vitamin D deficient.
See if there’s any other breakdown dark-skinned ethnic subgroups had much higher anywhere from three to 71 fold higher prevalence of serum 25 hydroxy vitamin D less than 30 nanomoles per liter, then did white populations. So here is a very interesting explanation that could be applied to the study that we just looked at in terms of mortality data in covid-19 is
we have this Baseline pandemic that was already there in 2016 based on the data in this study that showed that not only in general. Was there a significant vitamin D deficiency quote pandemic, but it was particularly exacerbated in dark-skinned ethnic subgroups according to this study.
So now let’s jump back ahead and look at some actual data that was published in mid April of this year regarding the role of vitamin D in the prevention of coronavirus disease and what they did in the study was pretty clever. What they decided to do was look at mortality rates of covid-19 in certain countries and compare it to the known mean value of vitamin D in that country in that population and amazingly they found a pretty good correlation. They say here in the
Active vitamin D levels are severely low in the Aging population, especially in Spain Italy and Switzerland. And this is also the most vulnerable group of the population in relation to covid-19. They say here it should be advisable to Forum dedicated studies about vitamin D levels and covid-19 patients with different degrees of disease severity.
Now in this table, you can see here the number of countries in Europe that were looked at 25 hydroxy vitamin D levels here in this column the cases of covid-19 and the deaths caused by covid-19 and we can go ahead and graph those and see what they look like.
And here are those graphs. Here’s the mean vitamin D level per country versus covid-19 mortality per 1 million population can see and that scattergram. There is a relationship. You can also see a similar relationship here with the mean vitamin D levels per country versus covid-19 cases per 1 million population.
One part of this article that I found interesting is that it actually shows that the pathology of covid-19 involves a complex interaction between the czar’s Cove to and the body’s immune system. It’s either that vitamin D or 125 dihydroxy vitamin D, which is the active form exerts a pronounced impact on ace2 and Angiotensin 1 7 access with enhanced expression of ace2. Remember this is the receptor for the SARS virus.
Ace2 is the host cell receptor responsible for median infection by stars Covey to from this perspective. It might be apparent that the risk of infection could be higher since you have more of these receptors. However, vitamin D has multiple roles in the immune system that can modulate the body’s reaction to an infection a boomer at all. I have described that vitamin D deficiency impairs the ability of macrophages to mature to produce macrophage specific surface antigens to produce the lysosomal enzyme acid.
Vitesse and to secrete hydrogen peroxide a function integral to their antimicrobial function
So because of these findings it’s been interesting to look in the literature about how honest scientists could disagree about whether or not we should wait for randomized controlled trials to come out to really tell us whether or not vitamin D. Supplementation is appropriate this point or whether or not we should just bite the bullet and everyone start taking vitamin D in the off chance that it might work and we get a head start on treating the population with vitamin D to reduce that high.
Amount of vitamin D deficiency as we saw a couple of Articles back.
I found this article that sort of goes through that debate in terms of whether or not we should take it or not. Take it reports arguing that high dose vitamin D supplementation could treat covid-19 are based on speculation and are a risk to Public Health warns a team of scientists from across the globe and it says here that scientists from the UK Europe and the United States including experts from the University of Birmingham have published a consensus paper in the journal bmj nutrition prevention.
Health warning against the use of mega-doses of vitamin D for preventing or treating the virus. They do note here that several studies published over the past couple of months have noted a link between vitamin D deficiency and covid-19 mortality with several concluding that daily supplementation could help reduce virus severity, but the current paper takes issue with reports concluding that doses higher than the safe Opera limit of four thousand international units per day could reduce the risk of Contracting the virus and
you successfully to treat it the report states that popular information channels such as social media platforms have been Rife with misinformation that has been perpetuated by fair and uncertainty. This has been the case particularly for diet and lifestyle advice.
Notes in particular one of those articles that says consider taking ten thousand international units a day of vitamin D3 for a few weeks to rapidly raise the 25 hydroxy vitamin D concentrations Then followed by five thousand international units per day.
They go on to say that the current study warns that calls to use high do supplementation to treat or prevent. The virus are without support from pertinent studies in humans at this time, but rather based on speculations about presume mechanisms, and the article goes on to talk about the debate basically between starting it now versus waiting for further tests. And I think that’s emblematic of the whole debate and just about everything that we’re trying to treat coronavirus with so I will leave it to you to read it and
With your own decision, I will add one footnote. And that is that when we reviewed this a couple of years ago in the British medical journal. It did say that one of the things that really was an indication of how well patients would do who took vitamin D. Supplementation is avoiding large doses at once and rather. It was the modest regular dosing of vitamin D that seemed to do the best in terms of reducing acute chest infections.
However, getting back to the question at hand. Is there a distinction between ethnic minority groups in terms of vitamin D levels and are they contributing to the disparity that we’re seeing in mortality? Well the way to answer that question of course is more studies and if it is true, then the inherent understanding would be that we would need to check what people’s levels are and customize their supplementation to their desired need.


Add comment