美国医学院讲师详细讲解急性肾衰竭的类型及成因三种。三种急性肾衰竭包括肾前衰竭,肾功能衰竭以及肾后衰竭。
Acute Kidney Injury: Pre-renal, Renal, & Post-renal and FENa-differential (Kidney Injury 3)
Okay, so welcome to another MedCram lecture. This is part 3 of acute renal failure. We’ve talked about BUN Creatinine and how to use it. I think that’s a good background for what we’re going to get into next and what we’re going to get into next is the different types of renal failure.
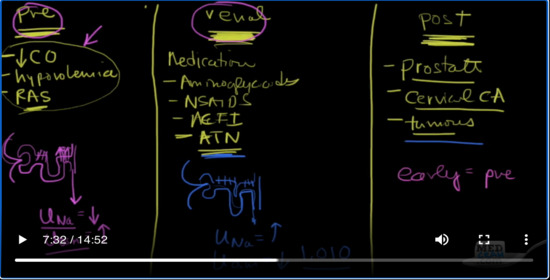
I’m going to kind of divide the screen into thirds. Okay, because there are three basic major types of acute renal failure and their aptly named. One is called prerenal failure, one is just called renal failure, and the other one is postrenal failure and we’re going to get into what these things mean. Okay, so you’ve got the kidneys, you’ve got blood coming to the kidneys and then the kidneys make urine and the urine goes out through the ureter down to the bladder, through the bladder and then out through the urethra and then outside.
So if there’s any obstruction from the ureter in the bladder and the urethra, that’s going to be a postrenal failure type of situation. If there’s any problem with the kidney itself. And I’m talking about the tubular cells, I’m talking about the
glomerulus, the tubular cells, the collecting tubule any of that stuff, then it’s renal. If there’s a problem with the blood getting to the kidney. So if you’re talking about congestive heart failure, renal artery stenosis, hypovolemia, hypotension any of that kind of stuff, you’re going to get a prerenal azotemia kind of situation.
So what are some things here that could cause prerenal? Let’s talk about prerenal first. So any kind of if there is decreased cardiac output, hypovolemia. Okay, how about renal artery stenosis, which is briefly Ras. So anything that prevents blood from getting to the kidneys is going to cause that.
What about renal? What causes renal problems? Well how about medications? There’s tons of medications that’ll cause renal failure. Let’s name a few. What about aminoglycosides? So those are antibiotics. What about NSAIDs? Okay. How about ACE inhibitors, ACEI. These are anti, these are hypertensive medications. So there’s a whole host of things. What about just necrosis, acute tubular necrosis. What’s acute tubular necrosis? Well, if there’s not enough blood reaching the kidney at first is you’re going to have a prerenal situation, but if that lasts for a long period of time, long enough like I mean by hours or a day, you can actually get something called acute tubular necrosis, where there’s just not enough blood that reach the kidney. There was no oxygen and the cells died. And usually this is a reversible situation, but you can certainly see ATN and so a lot of times what you’re going to be doing is trying to determine is this renal renal failure, in other words, it’s so bad that in other words was the hypotension so bad for so long that we have renal renal failure or it is just temporary enough that we’re dealing with prerenal failure.
We’ll talk about how you can figure out the difference between the two. Postrenal failure is pretty easy. The most common cause is just prostate. Okay, so a specifically in men the prostate is so large. It’s choking off the urethra and the bladder can empty and this backs up into the ureter and it causes what we call hydronephrosis. So this is water on the kidney, but there’s other things that can do this- cervical cancer. Okay cervical cancer can spread out to the ureter and cause an obstruction. Tumors, any kind of tumors out there or just anything that’s going to block the body’s ability to get rid of you, and kidney stones can do it. And so there’s several different ways that you can go into acute renal failure. So I you have to figure that out.
Okay so let’s concentrate for the moment on these two here- prerenal and renal, those are the two I want to concentrate on. So imagine your kidney and if you were in a situation like this, okay, imagine your situation your kidney and not enough flow is coming down the pipe, not enough blood is coming down to your glomerulus. Basically, you understand that as simply meaning that there’s not enough volume in the body. And so what are you going to do in this situation?
You’re going to want to hold onto as much salt and sodium as possible. And the reason is because volume in the body is determined by the kidney’s ability to reabsorb salt. And so if you’ve got your glomerulus, so I’m going to draw a little tiny nephron here. Okay, and you’ve seen this before no doubt. Okay. So you’ve got your afferent arteriole coming in and going out. You are going to make sure that every single tubal you’ll that you have at your disposal is reabsorbing sodium. Okay, so that’s going to be very important. And so that the urine that’s coming out. Is it going to be high in sodium or is it going to be low in sodium? Well, if you’re trying to take all the sodium out of that urine as much as possible and getting it back into the blood so your body can get more volume, you can bet that the urinary concentration of sodium is going to be low. Okay, but as the sodium goes, so does the water go with it. So sodium gets reabsorbed, water gets reabsorbed with it. What’s the concentration of your urine going to be?
So what’s the urine osmolarity? Osm. It’s going to be high. Does that make sense? So again, let’s review that. If you’ve got a nephron which is not getting a lot of flow, it is going to anticipate that you’re going to need more volume. And so it’s going to reabsorb sodium which is the key for getting volume. Sodium gets reabsorbed, water follows it, and so what you have is a low urine sodium because that’s what’s left. And what’s left is going to be very concentrated because all the sodium and the water is going to be taken out. And so you’re going to be left with all of the other things like their urea for instance and all the other things that the body gets rid of in the urine. So the concentration is going to be quite high. Now this is in contradistinction to what we see over here on the renal side.
Again, let’s go ahead and make glomerulus. Okay, here are the situation is different here. We’ve got the flow coming down. No problem, but the kidneys themselves, the tubular cells are not working. So if these tubules are not working, tell me, are they reabsorbing sodium and water? Answer is no, so they’re not. And so what are you going to see in the urine that passes by, you’re going to have urine sodium concentration is going to be high. Why is that because the cells are not doing their job. They’re not reabsorbing sodium like they should and as a result of that, water is not being reabsorbed. And so the urine osmolarity is going to be low and specifically it’s going to be around that of the serum and it’s going to be 1.010, otherwise known as Tenten. Okay, so high urine sodium, high urine osmolality. So we get over here to postrenal and what we usually see is that early on it appears as though it looks like prerenal. Okay, whereas later on, when the kidney actually starts to fail, it looks actually more like renal.
Okay. So let’s go over a couple of things that will show you how to determine how to figure out what’s going on with patients who come in with acute renal failure. Okay. So for postrenal failure, it’s pretty easy to figure that when a patient comes in. So for postrenal, what you do is you put a urinary catheterin. So if you catheterize the patient, put a catheterin otherwise known as a Foley catheter and a whole bunch of urine comes out and the patient’s relieved and the renal failure resolves. Then it was probably postrenal. So these are pretty easy to figure out you can get an ultrasound of the of the of the kidney. You could put a Foley in. There are several ways of figuring out where the problem is.
So if you remember the anatomy, you’ve got the kidneys. Okay, and you’ve got the ureters coming down. Okay, and they go into a bladder and then the bladder empties out until your urethra. So there’s several different places where you can have an obstruction. You can have it obstruction here in the ureter or you can have an obstruction here in the urethra. If you place a Foley catheter, which goes up the urethra and into the bladder and there’s a lot of residual there’s a lot of fluid in there and all of it comes out. Well, then you’ve got your answer. If you do it ultra sound, okay, and you see that these kidneys are large because there’s an obstruction here or down here. Then you can also make that determination as well. So ultrasound Foley catheter you can make the diagnosis of postrenal pretty well. Also if this patient has a history of prostate problems and it’s difficult to pass the Foley all of these are signals that what you’re dealing with here is a postrenal renal failure.
So I don’t want to focus too much on that because what you’re going to find most of your time trying to figure out is the difference between renal and prerenal. Okay. So let’s talk about prerenal versus renal. So we’re going to split the board here in two and we’re going to look at those. So let’s put prerenal up here, prerenal again is where the heart is not pumping enough blood or there isn’t enough blood or there’s a stenosis to the artery that’s going to the kidney. Basically, there’s a problem before the kidney or prerenal.
Okay, then let’s talk about renal over here. Okay. So let’s look at different categories. What about the urine osmolarity? So what we say here the urine osmolarity in prerenal is usually going to be greater than 500. Whereas in renal, it’s going to be less than 350. Why is that again? Because in prerenal you’re trying to hold onto sodium and water as much as possible. You’re trying to take every drop of sodium chloride and water out of that filtrate, and what you’re left with is a very concentrated urine. With renal on the other hand, your tubules are not working. And so as a result of that you’re letting stuff passed right through and so the osmolality or the osmolarity is very similar to that of blood and if you recall blood osmorality is around 295. So it’s going to be very similar to what you’re getting out of the kidney.
Another way of saying this is this is the specific gravity specific gravity. You’ll see in prerenal is usually greater than 1.010.The specific gravity and renal failure is about 1.010. In fact, we call it 10/10. This could get up as high over here by the way as 1.030 that’s pretty concentrated urine there. All right, so the other thing we can look at is we can actually measure the urinary sodium concentration. So the urinary sodium concentration, what do you think it’s going to be in prerenal? It’s going to be low. That’s right. So it’s going to be less than about 20. While it is in renal, you’re going to see usually greater than 40, you can actually order that as a lab and see.
What about sediment? Okay, what’s happening with sediment means sediment is simply dead cells from the kidney sloughing off and finding their way ending up in the urine. Would you expect to see sediment in a prerenal situation. Answer is no, you wouldn’t. Remember here. What’s the problem? The problem is there’s not enough blood and fluid getting to the kidneys. And as a result of that those cells, those very cells that were talking about. There are working overtime to try to get sodium chloride up. Now if they’re if this goes on for long enough, and is severe enough, the cells could die. Then you switch over and you become renal because when they die, the cells are not working anymore. And so they slough off and you do get positive sediments and that’s more of a regional phenomenon.
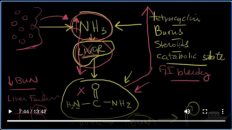
Finally, we get to the crux here and that’s the BUN/ Creatinine ratios. So what do we see with a BUN/ Cr. Remember in Prerenal, BUN gets increased because it’s not being filtered as much but it also goes up for another reason because it’s being reabsorbed, the proximal convoluted tubule. So typically our BUN/ Cr are greater than 20, whereas over here on the renal side they are usually less than or equal to 15. Now there’s one other thing that I would like to bring up and that’s something that you might see called the FENa. Okay FENa.
What’s a FENa? Well, let me let me clear the screen and show you the FENa is actually stands for the fractional excretion of sodium of the kidney. And the equation goes something like this. It is the concentration of sodium in the urine over the concentration of sodium in the plasma, all over the concentration of creatinine in the urine over the concentration of creatinine in the plasma. Complicated, yes!
But here’s the key thing. I want you to zoom in on and that is this factor right here. We’ve already said and you know this just algebraically that if this number is high that this number is going to be high, just algebraically. And so what kind of a type of failure causes you to have a high urine sodium concentration. Is it prerenal or is it renal? It’s renal because the cells are dead. So what you will see if we go back and split our screen here. We got prerenal and we got renal that if you’ve got a situation with a FENa. Okay, your prerenal is usually going to be less than 1.0 if you calculate this whole thing, okay, whereas with renal it’s usually going to be greater than 2 percent. Okay, these are both percents. It’s going to be lower in the prerenal because your urine sodium is going to be low in the prerenal. And why is that? Because the kidney is trying to reabsorb as much salt and water as possible.
Okay, so this concludes acute renal failure and how to interpret creatinine BUN those sorts of things. I thank you for joining me.


Add comment